Suprasellar salivary gland-like pleomorphic adenoma
2016-11-25 15:05 作者:三博腦科醫(yī)院
Kun Yao, Zejun Duan, Yu Bian, Mengyang Wang, Xueling Qi
ABSTRACT
Suprasellar salivary gland-Like pleomorphic adenoma is not a common disease and seldom reported so far. We are reporting a case of a 23-year-old man with recurrent suprasellar salivary gland-like pleomorphic adenoma, who underwent an operation of subtotal, subfrontal resection under the wrong pathology diagnosis of benign teratoma in another hospital 4-year-ago. Four years later, he was admitted to our hospital for additional visual loss of the right eye(left, 1.0; right, 0.4)resulting from tumor regrowth.Magnetic resonance imaging revealed that suprasellar extension and compressed optic chiasm resulted in visual disturbance of the patient. The tumor was totally excised and histological examination evidenced the pathological features of intrasellar salivary gland-like pleomorphic adenoma. The patient did not receive any further treatment and he is free from tumor recurrence for 30 months after the operation. From this point of view, clinical prognosis of intrasellar salivary gland-like pleomorphic adenoma was good after total surgical resection.
KEY WORDS: Central nervous system,pathologic findings, pleomorphic adenoma, suprasellarregion tumor
INTRODUCTION
The suprasellar salivary gland-like pleomorphic adenoma is not a common disease and seldom reported so far. We experienced a case of suprasellar salivary gland-like pleomorphic adenoma, which was misdiagnosed as pituitary adenoma in pre-operation.
CASE REPORT
Four years ago, a 23-year-old man visited a hospital with polydipsia, polyuria and signs of asymmetrical breast development and visual acuity loss of the right eye (left, 1.0; right, 0.6.) 4-year-ago.Radiographically, a large neoplasm with suprasellar extension was identified and thought to compress the optic nerves and chiasm. He had decreased cortisol,luteinizing hormone(LH)and follicle-stimulating hormone(FSH), and replacement therapy was initiated. His prolactin(PRL)was elevated;adrenocorticotropic hormone(ACTH), growth hormone(GH)and thyroid-stimulating hormone(TSH)were normal. Pre-operative diagnosis of pituitary adenoma was made on the basis of clinical features. Then he underwent an operation of subfrontal,subtotal resection under the pathology diagnosis of benign teratoma in that hospital.
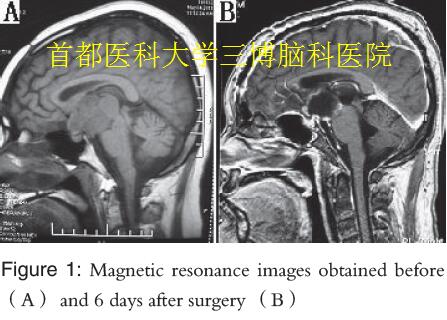
At 4 years later, he complained of additional visual loss of the right eye(left, 1.0; right, 0.4)and intermittent fever for 3 weeks resulting from tumor regrowth. He was admitted to our hospital for a second operation. The serum TSH decreased this time. PRL,GH, LH, ACTH and FSH were normal. Magnetic resonance imaging(MRI)revealed a large mass in the suprasellar region [Figure 1A]. The pre-operative diagnosis was either pituitary adenoma or benign teratoma this time. Craniotomy for tumor removal was performed through a right pterional approach.The tumor was gently removed completely from the hypothalamus and optic nerve.
The patient experienced uneventful recovery.He was well on replacement hormone therapy. MRI obtained 6 days after surgery showed the tumor was removed completely [Figure 1B]. The vision condition improved during the patient’s hospitalization period and he was discharged from our hospital 39 days after the operation.
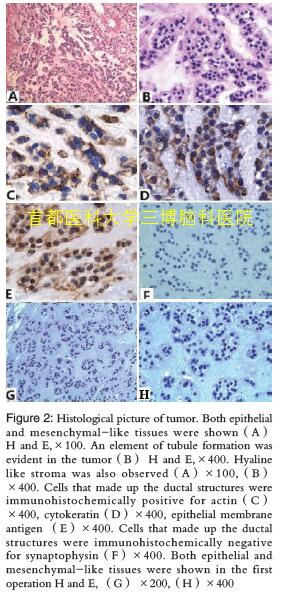
We obtained histological sections at the time of operation which were composed of both epithelial and mesenchymal-like tissues [Figure 2A]. Hyaline-like stroma [Figure 2A and B], and lots of myxoid stroma in the tumor [Figure 2A and B] were observed. We also found an element of vague tubule formation in the cellular portion [Figure 2B], occasionally some were composed of two layers of cells. The cells of tumor were uniform and cuboidal. Most of them were immunohistochemically positive for actin [Figure 2C], cytokeratin (CK) [Figure 2D], epithelial membrane antigen (EMA) [Figure 2E] and glial fibrillary acidic protein (GFAP), meanwhile negative for GH, ACTH, TSH, FSH, LH, PRL, synaptophysin (Syn) [Figure 2F]. The MIB-1 index of the tumor was 1.2%. From these findings, we made the histological diagnosis of suprasellar salivary gland-like pleomorphic adenoma.
DISCUSSION
Salivary gland-like tumor was an extremely rare non-adenomatous tumor specific to the sellar and suprasellar region. It had close relationship to the salivary glands resting in human posterior pituitary. Salivary gland rests have been reported in autopsy specimens. It was supported that the origin of salivary cells in the pituitary was from the epithelium of Rathke’s pouch. However, these tissues were considered as clinically silent. Occasionally, large lesions could cause hormonal abnormality, and might rarely give rise to salivary gland-like tumors in the sellar and suprasellar regions.
This tumor was easy to be misdiagnosed as pituitary adenoma in the pre-operation period.We knew many pituitary adenomas were either nonfunctioning or secreting hormones at such low levels that they became symptomatic only when they had grown large enough to produce visual symptoms resulting from compression of the optic chiasm and the normal pituitary. There were also many other tumors enter into the differential diagnosis of a sellar mass.These included craniopharyngioma, pituicytoma,granular cell tumor, meningioma, germcelltumors,malignant lymphoma, gangliocytoma, paraganglioma,hemangiopericytoma, metastatic tumor. Because pituitary adenomas were by far the most frequently occurring lesion, pituitary adenoma was always the first provisional diagnosis in pre-operation.
Many patients with sellar and suprasellar salivary gland-like tumors usually had similar clinical features such as visual disturbances, disorder of hormones levels and cranial nerve involvement. In this case,the clinical features included polydipsia, polyuria,disorder of hormones levels and visual acuity loss. On MRI, large masses of suprasellar region were found.Diagnoses were both pituitary adenoma at two times before operation. It was difficult to make completely correct pre-operation diagnosis merely by clinical history and MRI findings.
We thought the differential diagnosis relayed mainly on the basis of histopathological and immunohistochemical findings. The diagnosis of suprasellar salivary gland-like pleomorphic adenoma was made on the basis of positive immunostaining for CK, EMA, GFAP, the well-differentiated cells with a moderate MIB-1 labeling and the glandular structure.In our case, the tumor cells were positive for CK, EMA and GFAP, but negative for GH, ACTH, TSH, FSH,LH, PRL and Syn. In combination with the hyaline-like stroma structures, the tumor was diagnosed as salivary gland-like monomorphic adenoma of the suprasellar region. We got embedded paraffin sections from his first operation 4-year-ago. Both ductal structures and mesenchymal-like tissues were found in the first specimen [Figure 2g and h]. Hence, microscopic structures indicating the diagnosis of teratoma was indeed wrong 4-year-ago.
In this case, the tumor was not totally resected in his first operation due to a wrong diagnosis of benign teratoma in other hospital 4-year-ago. We thought incomplete removal was the important reason for relapse. Recurrence of pulmonary artery following surgery was recorded in some reports rising to 44%.Incomplete excision of the tumor was considered as the only proven reason contributing to recurrent disease.This is why a complete resection of the mass was performed in the present case. Options for pleomorphic adenoma of salivary gland treatment included both operation and radiotherapy. Whereas some studies had reported enhanced local control with post-operative radiation therapy compared with surgery alone, others had found no significant improvement in outcome. We found Gamma knife radio surgery not only failed to control the tumor but also changed a prominent portion into degenerated tissue. Hence in the present case, we did not advise the patient to have radiotherapy. The patient is free from tumor recurrence after operation for at least 30 months.
(參考文獻略)



 京公網安備 11010802035500號
京公網安備 11010802035500號